Educational Guide Specializing in “Gulf War Illness”
We are working on the update do to many law changes in the past year.
NGWRC is funded only by donations
NGWRC is a 501(c)3 non-profit organization, and your donations are tax deductible. Our paperwork is on file with the state of Kansas and if you need a copy you can get it from the Secretary of States' office. The NGWRC reserves the right to refuse donations from any groups or persons whos' views does not support ours.
Undiagnosed Illness Claim (UDX)
CHAPTER II
This chapter will cover only the undiagnosed illness part of the law as found in [38 CFR §3.317(a)(2)(i)(A)] and the symptoms as listed in §3.317 (b). There is a new regulation veterans need to use in there claim 38 CFR §3.320. Alwas look at the law par too. 38 U.S. Code §1117 - 1120.
This guide is only our views of how to prepare a claim, but it comes from working many claims, helping veterans and their VSO’s, and reading court cases.
You need to work closely with your power of attorney (POA), (service officer, agent, or lawyer) when doing any type of claim, but this types of claims or even more so. That is why we have been telling veterans to always ask around about the service officers in their area. You need to find the one that knows this issue and has worked it and won.
Winning this type of claim can come down to simple wording that you used in your statement to support your claim or that you say in your C&P exam that does lead to the granting or denial of the claim. The wording can set the level of the rating.
When is a symptom not an undiagnosed illness?
You cannot file for sleep apnea, Diabetes Type I or Type II, Multiple Sclerosis, and GERD under this law. They are not presumptive illnesses. Some of these are addressed in the rule-making found in the federal register and some in the 38 CFR 3.317. Congress addressed some and that is why you will see them in the Jun 10, 2003 rule making.
This guide should help you start a claim for disability compensation for Undiagnosed Illness (UDX) or a claim for a CMI that may be caused by your service in the Gulf War. At the same time, this guide may help you to decide if your symptoms are secondary to (caused by) the medication you take for a disability you now have or one which is an undiagnosed illness. With a secondary issue and a doctor’s nexus and research, you would file on that basis and would have a better chance of winning a claim.
You need to make sure that before you file a claim for a UDX that you really have an undiagnosed illness as per the law and not symptoms that can be related to a diagnosed illness or a diagnosed chronic multi-symptom illness.
A claim for a UDX is the hardest type of claim to do, and most of the time you need to plan on going all the way to the Board of Veterans' Appeals (Board) and even to the United States Court of Appeals for Veterans Claims (Court or CAVC).
The VBA (examiner) will be looking at everything that you are diagnosed with to see if any of it can cause the same symptoms. This is in keeping with the law passed by Congress; if the symptom can be assigned to a known cause at the time, then it cannot be an undiagnosed illness. This is concluded by means of testing. Decisions are not always satisfying, however. Sometimes the examiner will “overreach” in writing the medical opinion or give a medical opinion that has no medical rationale or facts to uphold it. Other times, the opinion will show the examiner does not understand the field they are talking about. These are the times you need to point out the inadequate exams.
We have seen problems where veterans did have many symptoms in their records that they file for and the Gulf War General Medical examination will show “no” to most of them anyway. In those cases, the examiner may not have read the veteran’s statements or the research the VSO sent in with the claim. Each one of these can make the exam inadequate.
There are a number of diagnosed illnesses that share the same symptoms. If you have a diagnosed illness with a known or partially understood etiology, it can prevent the granting of the claim for a UDX claim. An example is headaches. The VBA may say that if you are diagnosed with migraine headaches, you do not have an undiagnosed illness. Fortunately, a claim is not lost on this issue if the VSO uses the VA’s 30,000 person study that showed the deployed veterans had migraines at a much higher rate than non-deployed veterans[1].
The same is true for a veteran who has had a heart attack or coronary artery disease. While the symptoms are listed under the law for the undiagnosed illness, you now have a diagnosed illness that the symptoms are caused by, and thus you are not able to file under 3.317. As such, a claim under 3.317 for the symptoms will be denied.
If you have a diagnosed medically unexplained chronic multi-symptom illness (MUCMI) such as Chronic Fatigue Syndrome, Fibromyalgia, Irritable Bowel Syndrome, TBI or a functional gastrointestinal disorder (FGID), please read and use the sections for those specific diagnosed illnesses. You should remember that all undiagnosed gastrointestinal problems can now fall under the FGID. All FGID’s are commonly characterized by symptoms including abdominal pain, substernal burning or pain, nausea, vomiting, altered bowel habits (including diarrhea, constipation), indigestion, bloating, postprandial fullness, and painful or difficult swallowing with no known cause.
Filing for undiagnosed illness at the same time you file for other claims with the same symptoms will delay them, but the VBA is now deferring the claims to speed up some decision. That is, if you are diagnosed with Fibromyalgia, you should only file for that illness and not the subpart of fatigue, muscle or joint pain, memory issues, and sleep disorder. The law does not allow for it. If you have a diagnosis for the MUCMI’s, you cannot file for the symptoms, too. See Table:
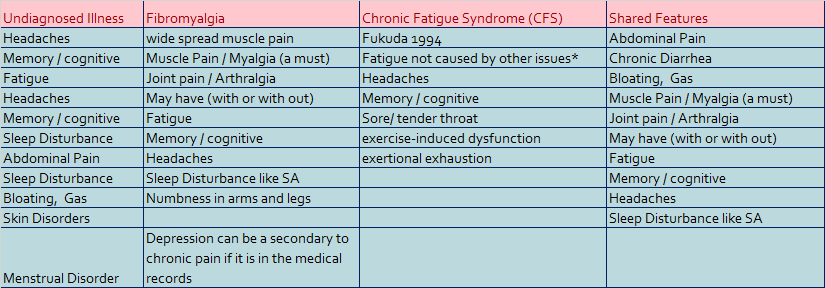
As you can see in the table the only symptoms that are not related to the three presumptive is the skin disorder and the menstrual disorder. Both would still need to be of unknown causes for you to file under section 3.317. The table below is only an example as there are many other illnesses you can be diagnosed with that will prevent (deny) a claim for UDX. Some of the issues can be claimed as a secondary to things you might have granted such as sleep apnea as a secondary to you treatment for your PTSD and fibromyalgia.
|
You have this symptom |
You cannot claim a UDX if diagnosed with |
|
Chest pain |
GERD, Heart Attacks/ myocardial infarction (MI), COPD, Neuro |
|
Fatigue |
PTSD / mental Health, Medication, Sleep Apnea, anemia, thyroid disorder. |
|
Memory / cognitive |
PTSD / mental Health, Medication, TBI |
|
Sleep Disturbance |
PTSD, Sleep Apnea, Insomnia, Narcolepsy, Restless Legs Syndrome, Shift Work |
|
Joint pain |
Arthritis, such as rheumatoid arthritis and osteoarthritis, DJD infection, and extremely rarely it can be a cause of cancer of the joint. |
|
Skin Disorders |
Less than 5% of the body/expose area. Of a known cause, fungal, bacterial, or parasitic (plant or insect) |
Preparing a claim for an undiagnosed illness
Any claim under 38 CFR § 3.317 can be very hard, but a claim for undiagnosed illness can be one of the hardest. Some veteran service organization representatives (VSO reps), agents, and lawyers have a hard time preparing these claims and working an appeal if it becomes necessary. That is why you, the veteran, will need to get a lot of paperwork done to help your POA with your claim --even more than in most claims. The veteran is the one who knows the times he/she went to the doctor’s office for the symptoms, and he/she is the only one who can write about the symptoms and how they are affecting his/her life. If you went to non-VA doctors, you must get the records, fill out a VA Form 21-4142a, and list all of the doctors that have treated your symptoms since the service.
Use the information in this chapter to help prepare a claim for undiagnosed illness or for specific symptoms which have not been associated with any diagnosis.
If you have a diagnosed illness with the same symptoms and it is not a medically unexplained chronic multi-symptom illness as outlined in the regulation, then you should file under a different section of VA regulations. You may or may not have a 38CFR§ 3.317 (a) claim for presumptive service connection.
Key elements that should be established in your claim
Due to some law changes, some forms are not use and we are working to update this guide
To receive compensation for an undiagnosed illness due to your service in the Gulf War, you will need to include/prove some of the following to the VA:
- US military service in the Southwest Asia Theater between 2 Aug, 1990 and the current date*.
- You have an undiagnosed illness of some type. (You cannot just claim “Gulf War Illness.”)
- You have “Objective Medical Evidence” as per § 3.317(3)
- Records from work showing time lost due to the symptoms you have.
- A detailed statement from you on the symptoms. See section on Form 21-4138.
- A detailed statement from others that have firsthand knowledge of you and your conditions(s) and service.
- All medical records for the symptoms that the doctors could not diagnose.
Use your DD214, and have your VSO or the VA certify it before THEY fax it to the VA Regional Office (VARO). Also, send in a 21-4138 stating what unit you were in. You may say: B Btry, 4th BN 5th FA, 1st ID, Ft. Riley Kansas, but it may be better if you did it like this: 2nd Battalion of the 505th Parachute Infantry (UIC WABVA0). If you are submitting a claim for PTSD, it may be best to reference the UIC on the orders sending you to and from the unit and theater of operations. Sometimes claimants are told they were not in the Gulf War, and this attention to detail will help stop that. Remember you are working to win at the VBA and/or BVA.
Why do I need that?
You need to understand what it takes under the regulation of presumptive to be granted a claim. Below is the wording from the case of Gutierrez v. Principi, 19 Vet.App. 1 (2004)[2], slightly changed so it is in line with the regulation as of today’s date:
Section 1117 of title 38 of the U.S. Code provides for entitlement to compensation on a presumptive basis to a Persian Gulf War veteran who complains of having an undiagnosed illness or illnesses that are 10% or more disabling during the presumption period established by the Secretary. 38 U.S.C. 1117(a)(1)(A) and (B). Pursuant to section 1117(d)(2), the Secretary has promulgated 38 C.F.R. 3.317, which provides, in pertinent part: (a)(1) Except as provided in paragraph (a)(7) of this section, VA will pay compensation in accordance with chapter 11 of title 38, United States Code, to a Persian Gulf veteran who exhibits objective indications of a qualifying chronic disability, provided that such disability:(i) Became manifest either during active military, naval or air service in the Southwest Asia theater of operations during the Persian Gulf War, or to a degree of 0[%] or any time after the service (2022 PACT Act change); and (ii) By history, physical examination, and laboratory tests cannot be attributed to any known clinical diagnosis.[3]
Manifestations of undiagnosed illnesses are presumed service connected unless there is affirmative evidence that an undiagnosed illness was not incurred in service or was instead caused by a supervening condition. See 38 C.F.R. §3.317 (a) 7. What this means is that you cannot have had the symptoms before you deployed. It also means that, after you came home, something could not have happened that could cause the same symptoms. This is where veterans using these pilot studies can be harmful to their claims for undiagnosed illness. If someone tells you that a pilot study shows your illness is caused by “X” due to Dr. Z’s study, and then you tell your doctor or VSO, the VSO inputs it into your file. Your claim for undiagnosed illness will more than likely be denied because your symptom now has a known cause. The law is clear that once you have a known cause, you cannot be given a grant under § 3.317; that is, unless you use the large studies and the benefit of the doubt rule with a good nexus statement.
Thus, in order to establish service connection under 38 U.S.C. §§1117, 1118, and 38 C.F.R. §3.317, a claimant must present evidence that he or she is a Gulf War veteran who:
(1) Exhibits objective indications;
(2) Of a chronic disability such as those listed in paragraph (b) of 38 C.F.R. §3.317;
(3) Which became manifest either during active military, naval, or air service in the Southwest Asia theater of operations during the Gulf War (note: in the gulf), or to a degree of 0% and
(4) Such symptomatology by history, physical examination, and laboratory tests cannot be attributed to any known clinical diagnosis, except a diagnosed medically unexplained chronic multisymptom illness. 38 U.S.C. §1117; 38 C.F.R. §3.317(a).
If you are working on a CUE claim because your claim was denied before August 10, 2022 the one thing that many veterans need to remember is that their symptoms need to meet the 10% rating level before the VBA will grant a service connection on a presumptive basis. This means that you can have everything in the records to prove the claim, but it may not meet the 10% disabling rating in the regulation. There is a court case on this with a GW veteran who has a diagnosis of Fibromyalgia (FM). He refused any treatment for it, so he was not granted his claim. The 10% level of FM requires some type of treatment, and each level depends on how well the treatment works. On a direct basis, a veteran can get a 0% rating. A VSO rep can assist with likely ratings as your prepare your claim.
This has always been the one part of the claims file that the VBA does incorrectly if the raters are unaccustomed to GWI. The difficulty is that there are so few of these claims and the standards for this to be used are lower than in most every other type of claim. Very few claims use the time lost from work or the seeking of treatment with no diagnosis. You need to make sure the examiner addresses it right for an adequate exam, too.
To have a better chance of winning, you need to include objective medical evidence in your claim from the start. If you are on the appeal, you can work and get it in now. The medical reports and work reports are the most important ones. For every doctor and hospital you went to that is not a VAMC, you will need to fill out a VA Form 21-4142. Work to get the records yourself, too. That is because if the doctor’s office asks the VA to pay anything for a copy, the VA will not, and those records will therefore not get in your file. You will get a letter telling you this and asking you to get the records. Often the VBA will then deny the claim and tell you that you have one year to get the records. You are now behind the eight ball if you let this happen. So get the records first. That is why you filed the “intent to file” in the first place – to buy yourself the time to do this kind of work. You will need to address these records in your VA Form 21-4138. This will help your claim and will make your statement look much better. It will guide the rater over the history of your illness, if he reads it. The examiner is to read this information, too, although most do not. This is where you can find an error in the claim, and the exam can become inadequate.
This is what the law calls for.
"Objective indications of chronic disabilities" include both "signs" in the medical sense of objective evidence perceptible to an examining physician and other, non-medical indicators that are capable of independent verification. Non-medical indicators include, but are not limited to, such circumstances or events as time lost from work, evidence that a veteran has sought medical treatment for his or her symptoms, and evidence affirming changes in the veteran's appearance, physical abilities, or mental or emotional attitude. As you might have noticed, we used the wording from the Federal Register. That is the only place you will find how some of the terms in the regulation are defined. It is how VBA and/or Congress meant to use it, and it is sometimes best to use the Federal Register in your appeal for the intent of the regulation.
Lay statements (VA form 21-4138) from individuals who establish that they are able from personal experience to make their observations will be considered as evidence if they support the conclusion that a disability exists. Objective indications will assist in determining both the actual presence of a disability and the extent of impairment caused by the disability. Some of the best statements come from the veteran’s (ex) employer/supervisor(s) and (ex) spouse.
List your signs and/or symptoms, and separate out those which are undiagnosed
List out each of the symptoms that you have; a computer spreadsheet will work the best for this. As you list each symptom, include the date it first appeared or when you went to the doctor. The history section does have the list if you need to look back, but you will find it is best to be using your medical file, since it will have a list of signs and symptoms. Once you have all of your symptoms listed, sort out those which are undiagnosed and those which are part of a diagnosis. Some symptoms may be a part of a CMI, PTSD, or some other illness like GERD, sleep apnea (SA), Major Depression Disorder (MDD), Crohn's Disease, cancer, coronary heart or artery disease -- to name a few. Your doctor or nurse may be of some help here. You need to remember that CMI’s of partially understood etiology and pathophysiology, such as diabetes and multiple sclerosis, cannot be claimed under this section, nor can you claim any of their symptoms.
If you have a diagnosis, such as Chronic Fatigue Syndrome (CFS), remember to list only those symptoms which are not CFS (or any other diagnosis) in your claim for undiagnosed illness. You may claim both the CFS and the completely undiagnosed symptoms, but they are separate issues in the VA's eyes. If you confuse the issues in your claim, you may delay your claim, or the VBA may combine everything under one claim. It may even increase your chance of being denied. CFS does have a lot of symptoms under it.
There is a presumptive end-date for the last date for your symptoms to manifest or to be reported in medical records. That date is now December 31, 2021 for the symptoms to manifest, but you may file your claim after that date as long as you have a record of symptoms appearing earlier than December 31, 2021. You need to go to the doctor to find out what is causing the symptoms as a part of the claim. You need to ensure this is for more than six months and that the doctor is doing tests to rule out other illnesses. For example, while a skin disorder of unknown causes accrue at higher rates you need to make sure that your doctor runs tests on the rash and doesn’t just do the “look and say” type of DX (diagnosis). The other aspect you need to understand is there are many medical terms used to describe a skin rash, but the courts and the FR have said that you need to be diagnosed. A descriptive term is not a diagnosis. [4]
It is important to remember that in the Federal Circuit, Joyner v. McDonald, 766 F.3d 1393 (Fed. Cir. 2014) held that a medical professional does not have to have eliminated all possible diagnoses before the veteran can be compensated for a disability due to an undiagnosed illness. Refer to the Claims 101 chapter for details related to filing your claim and forms needed.
Critically Important Claims Protocol
Sometimes veterans have both diagnosed and undiagnosed symptoms which can be claimed under §3.317(a). Once a symptom is established and claimed as a diagnosed illness, it may no longer be claimed as part of an undiagnosed illness. Some of the diagnosed conditions may still be claimed due to the exposures you had. This is where the large VA studies will work for you. Remember that the pilot studies will not work in a claim; only large peer reviewed studies maybe helpful. See the Claims 101 chapter. This will only work in some cases; it is only appropriate on a case-by case bases.
What this means is that if you wait to file a claim for undiagnosed sleep disorder and your records show that you do have a clear diagnosis of sleep apnea, the claim will not be granted. The VBA will tell you that your undiagnosed sleep disorder is denied because this disability is determined to result from a known clinical diagnosis of sleep apnea. The same thing will happen if you file for headaches and have in your records a diagnosis of migraines. A diagnosis of tension headaches should give a reason; sometimes they can be claimed as secondary.
In the example above, you do not have a claim under §3.317 for an undiagnosed sleep disorder, and you cannot file the sleep apnea under §3.317. It is a diagnosed illness and not a presumptive illness under this section of the regulation. There is an article on the NGWRC website on sleep apnea as a secondary to medication side effects for mental health. VSOs will need to use the VA 2005 study found there, too. Make sure your VSO rep reads this article before you try to file a claim.
Sorting out your symptoms and your diagnoses is very important in building a strong claim for compensation under §3.317(a)(2)(i)(A). If you have a medically unexplained CMI diagnosis, you need to file for that. The CMI claim is not as hard to get granted has a UDX.
You will also need to look at secondary service connection for some of your symptoms. This is often overlooked by veterans and their POAs. A simple example is a veteran with a right knee and right foot injury that he is rated for. Over the years, his hip goes out due to the poor walking from the right leg injury as per his medical files. He can now be granted service connection for this on a secondary basis. This is what the website on sleep apnea is talking about.
Many veterans have a problem with GERD. One of the reasons that I feel that such GW vets have GERD is all of the medications they are on[5]. See the NGWRC write-up on sleep apnea that is on the website.
In addition, skin disorders, chest pain, heart palpitations, abnormal weight loss, menstrual disorders, and any other symptoms that fall under the thirteen signs and symptoms should be explained and defined to the best of your ability before you begin this type of claim.
Please remember that each symptom must be a 'medically unexplained symptom' in order to qualify you for compensation under 38 CFR §3.317(a)(2)(i)(A). Other medical diagnostic terms with similar meaning to 'medically unexplained' are 'functional', 'somatoform', and 'idiopathic.' If your doctor uses any of those words to define the cause of your symptoms, or to diagnose them, they are usually 'medically unexplained.'
As you prepare your claim, remember to list all your symptoms which fall under these categories and each diagnosis. Match up the symptoms to the diagnoses you have so that you don't include a 'diagnosed symptom' in a claim for undiagnosed illness. If you also have a Traumatic Brain Injury (TBI) or a Post-Traumatic Stress Disorder (PTSD) diagnosis, consult with your doctor and your VSO rep about where to assign overlapping symptoms which may result from more than one of those causes. You may be able to list symptoms under more than one diagnosis, but you may never list those same symptoms as ‘undiagnosed.’ If you were diagnosed with Type 2 diabetes before filing under this section, be aware that most undiagnosed symptoms will be ruled out.
While the VA is denying many of the claims unjustly, you need to make sure to file them correctly. With the many years of helping veterans, we have developed an example for you to use on one type of claim.
Here is an example for a veteran:
Diagnoses the veteran has
Chronic Fatigue Syndrome (CFS)
Irritable Bowel Syndrome (IBS)
Undiagnosed symptoms
Symptoms the veteran has
Unrefreshing sleep CFS
Multi-joint pain without swelling or redness CFS
Muscle pain CFS
Daily Cramping IBS
A sore throat that is frequent or recurring CFS
Significant impairment of short-term memory/ concentration CFS
Diarrhea some days IBS
Constipation other days IBS
Bloating IBS
Mucus in stool IBS
In the above case, the claimant has been diagnosed with CFS and IBS. The claimant would file for both issues using the Gulf War regulation 38 CFR §3.317(a)(2)(i)(B). The claimant will not file a claim for symptoms related to either CFS or IBS. The claimant will make a total of two claims: CFS and IBS due to his service in the Gulf War as per 38 CFR §3.317(a)(2)(i)(B). It is important that this wording is together with these illnesses on your 21-4138 for each illness.
Remember: adjudicators are not doctors, and these are unusual claims; medical examiners do not make legal rulings like determining if a condition is a presumptive. The examiner is to tell the Compensation and Pension (C&P) adjudicator only what is asked of them. Do not bring the ‘Notice to the Examiner’ to your exam as the examiner already has it in your file. If you MUST be diagnosed with the CMI before, you file and before the exam, bring the diagnosis and the testing that was done -- especially if it was outside of the VA. You can dispute the exam in your NOD. Remember no matter how nice comp & Pen examiners are during your examination seem, they are not your friends and most likely do a poor job on your exam. Be honest and frank with them. They are told to be nice. They are doing their jobs.
Make sure your VSO cover letter addresses the regulation that your claimed illness falls under, such as that it is a presumptive illness under §3.317(a)(2)(i). If you don't help them find the information they need to resolve your claim fairly, there is a good chance they won't. It is your VSO rep who will be able to talk to the rater right away if something goes wrong, but only if he is in the loop. Keeping the VSO reps at the VARO in the loop is what you need to do; they are the only ones working the claim for you, unless you have a claims agent or lawyer. On occasion, VSO reps have left this wording out, and valid claims were subsequently denied. Remember that a problem with some GW vets is their cognitive skills due to their illnesses, so please work with your VSO rep.
After you have listed each diagnosis, continue with individual symptoms which are undiagnosed. Each of the undiagnosed symptoms is filed in a similar fashion. “I am filing a claim for my chronic diarrhea as a presumptive service connected disability due to my service in the Gulf War per 38 CFR §3.317(a)(2)(i)(A), and it may also be a CMI under §3.317(a)(2)(i)(B)(3). The Form 21-526b (claim for disability compensation) will let you list each symptom due to the Gulf War, but you will need to also fill out a 21-4138 (statement in support of claim) and list out each of your symptoms in a statement. Fill out a separate 21-4138 for each symptom so the raters can track that symptom better.
[1] Kang HK, Mahan CM, Lee LY, Magee CA, Murphy FM. Illnesses among United States veterans of the Gulf War: A population-based survey of 30,000 veterans. Journal of Occupational and Environmental Medicine. 2000;42(5):491–501.
[2] Gutierrez v. Principi, 19 Vet.App. 1 (2004)
[3] 60 FR 6665, Feb. 3, 1995, as amended at 62 FR 23139, Apr. 29, 1997; 63 FR 11122, Mar. 6, 1998; 66 FR 56615, Nov. 9, 2001; 67 FR 78979, Dec. 27, 2002; 68 FR 34541, June 10, 2003; 71 FR 75672, Dec. 18, 2006; 72 FR 68507, Dec. 5, 2007; 75 FR 59970, Sept. 29, 2010; 75 FR 61356, Oct. 5, 2010; 75 FR 61997, Oct. 7, 2010; 76 FR 41698, July 15, 2011; 76 FR 81836, Dec. 29, 2011; 77 FR 63228, Oct. 16, 2012
[4] NEGRON-JIMENEZ v. SHINSEKI October 21, 2009 I use this single judge ruling as it brings out the skin issue in a GW-claim.
Updated November, 2017 V3.0
Distribution and Disclaimer
Gulf War Illness (GWI) is a generic term for a variety of medical problems which will be discussed in detail. This guide is not a review of the protocols for medical treatment of GWI; that goal is all too elusive. The primary purpose of this guide is to assist the veteran -- who believes he or she is afflicted with GWI -- with procedures for filing a claim for disability with the Department of Veterans Affairs and enhancing the probability of success in that endeavor.
Gulf War Illness is not something you can claim under 38 USC 1117. GWI is only a term to describe the symptoms veterans have from their service in the Gulf War. The VA and DOD are working on a case definition for it to be diagnosed as medically unexplained chronic multi-symptom illness, but this has not happened yet. It should be done soon.
The contents of this guide are for informational purposes only. Every effort is made to achieve accuracy, but neither the National Gulf War Resource Center, Inc. nor its principals assume responsibility for the accuracy or veracity of the information contained herein.
This guide is distributed freely to veterans, Veteran Service Organizations, accredited VA Agents, lawyers, and others interested in helping those who are ill, injured, or disabled due to the Gulf War. Any other use requires the written authorization of the National Gulf War Resource Center (NGWRC) or sources used in this guide.
Thank you one and all,
James A. Bunker, Executive Director & VA Accredited Claims Agent.

